Abstract

Myeloid/lymphoid neoplasms associated with eosinophilia (MLN-Eo) and tyrosine kinase fusion genes include rearrangements of PDGFRB with over 30 different partner genes, most commonly ETV6-PDGFRB. Rearrangements are evident by cytogenetic analysis and fluorescence in situ hybridization (FISH) break-apart probes. Herein, we describe a novel rearrangement partner for PDGFRB.
A 25-year-old man with a medical history significant for gout and hypertension presented to medical care after several days of progressive dyspnea, chest pain, fatigue, epistaxis, and rash. Physical exam revealed palpable cervical, axillary, and inguinal lymphadenopathy and massive splenomegaly. By CT scan the spleen measured 25 cm and diffuse lymphadenopathy was identified in the chest, abdomen and pelvis with the largest lymph node mass measuring 8.9 x 2.5 cm. Transthoracic echocardiogram showed normal heart function and no evidence of myocardial injury. The patient subsequently developed respiratory failure requiring intubation and mechanical ventilation, shock requiring vasopressors, and renal failure requiring renal replacement therapy. Initial laboratory evaluation demonstrated a leukocytosis to 83.3 x 10 9/L with neutrophilic predominance with left shift and eosinophilia (10% of WBCs, absolute eosinophil count of 8.2 x 10 9/L); hemoglobin of 8.3 g/dL and hematocrit of 25%; and thrombocytopenia to 50 x 10 9/L. Ferritin was 660 ng/mL, lactate dehydrogenase 384 U/L, and uric acid 10.4 mg/dL. Secondary causes of eosinophilia including infection, immunodeficiency, atopy, medications, and rheumatologic disease were ruled out. The patient was positive for strongyloides IgG antibodies and received ivermectin.
Core biopsy of a lymph node was non-diagnostic and could not repeated safely due to progressive severe thrombocytopenia. Skin biopsy demonstrated a perivascular leukocytoclasis, but no abnormal B or T cell population. Bone marrow aspirate and biopsy revealed a hypercellular marrow (90%) with mild trilineage dysplasia, granulocytic hyperplasia, moderate reticulin fibrosis, and slightly increased mast cells. Blasts were not increased and no hemophagocytic histiocytes were identified. Eosinophils accounted for 6.9% of myeloid cells. Flow cytometry did not reveal an abnormal B or T lymphoid, blast or myeloid population.
Peripheral blood flow cytometry did not reveal an abnormal B or T-cell population and T-cell rearrangement studies showed an oligoclonal population. No clonal B cell population was identified.
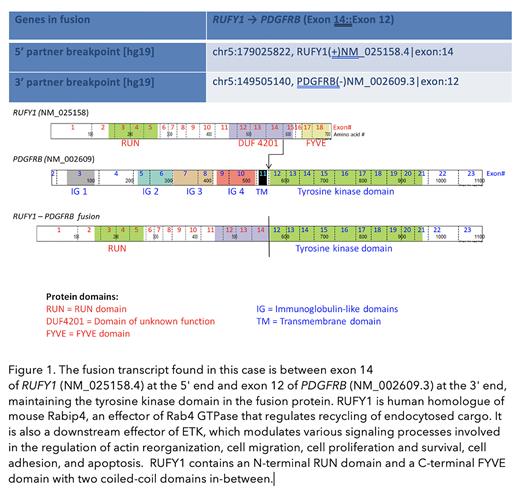
FISH, which identified a rearrangement of PDGFRB in 28% of cells, confirmed the diagnosis. Karyotype analysis revealed an abnormal male karyotype with a paracentric inversion of 5q with breakpoints at 5q32 and 5q35. FusionPlex® Solid Tumor Panel (Clinical Genomics Laboratory, University of Washington SOM) identified a novel fusion between RUFY1 and PDGFRB. RUFY1 is expressed in most tissues and encodes a protein that contains a RUN domain and a FYVE-type zinc finger domain and plays a role in early endosomal trafficking (Figure). We are currently demonstrating the fusion is oncogenic and sensitive to tyrosine kinase inhibition in Ba/F3 cells. The patient's remarkable clinical response, however, supports imatinib sensitivity and is in keeping with other published reports of MLN-Eo with PDGFRB rearrangements. Initial treatment included high dose steroids for 7 days and hydroxyurea briefly. Imatinib 400 mg daily was started, then decreased to 200 mg daily due to gastrointestinal toxicity. Follow-up is limited (8 weeks). However, the patient has recovered clinically. Six weeks after starting imatinib he had renal recovery and has achieved a complete hematologic response except for mild anemia due to resolving acute kidney injury. Splenomegaly and peripheral lymphadenopathy have resolved. PDGFRB FISH has declined to 9%.
Inversions of chromosome 5 have very rarely been described in association with eosinophilia, but only one report has specifically identified a rearrangement of PDGFRB. This report described a novel rearrangement involving exons 12 to 23 of PDGFRB at 5q32 and the 5′ (UTR) of G3BP1 at 5q33.1. Notably, this specific rearrangement was undetectable by PDGFRB break-apart FISH. These reports and ours highlight the clinical relevance of NGS in identifying novel rearrangement partners. Furthermore, patient-specific ddPCR assays can be designed for sensitive monitoring.
Oehler: BMS: Consultancy; OncLive: Honoraria; Pfizer: Research Funding; Takeda: Consultancy; Blueprint Medicines: Consultancy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal